-
×
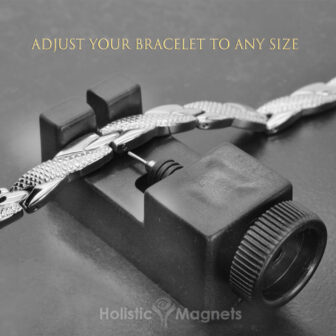 Bracelet Adjustment Tool
1 × €4.99
Bracelet Adjustment Tool
1 × €4.99
Subtotal: €4.99
 Osteoarthritis is the breakdown of cartilage, a spongy protein that covers the ends of the bones within a joint. Normal cartilage helps with shock absorption by serving as a cushion at the ends of the bones. The cartilage as the fluid within the joint allows for smooth joint movement. As osteoarthritis progresses, the space between the bones narrows, the cartilage wears down and the underlying bone is exposed. This results in painful movement of the joint as well as limited motion. Bone spurs can develop around the joint, limiting motion further and contributing to more pain. Inflammation plays only a minor role in osteoarthritis.
Osteoarthritis is the breakdown of cartilage, a spongy protein that covers the ends of the bones within a joint. Normal cartilage helps with shock absorption by serving as a cushion at the ends of the bones. The cartilage as the fluid within the joint allows for smooth joint movement. As osteoarthritis progresses, the space between the bones narrows, the cartilage wears down and the underlying bone is exposed. This results in painful movement of the joint as well as limited motion. Bone spurs can develop around the joint, limiting motion further and contributing to more pain. Inflammation plays only a minor role in osteoarthritis.
There are many causes of osteoarthritis, the most well known is the aging process. As we age, the water content of cartilage increases and the protein content decreases. As the water content increases, the cartilage becomes softer, more permeable and loses it’s mechanical properties. The protein content decreases which contributes to slow degeneration of the cartilage, resulting in flaking and erosions.
Other causes of osteoarthritis include abnormal bone alignment. In the foot, the most common cause is faulty foot mechanics. When the foot is not in alignment and not functioning properly, this causes abnormal stress on joints in the foot, ankle, knee, hip and back. Trauma is a well known cause of arthritis. Direct trauma can disturb the joint structures, cause mal-alignment of the joint or cause weakness of the surrounding structures, resulting in instability of the joint and eventual osteoarthritis. Other causes, such as infection, medications (such as steroids) and genetics contribute to the development of arthritis.
Obesity is a common cause of arthritis. The exact mechanism of how excess weight influences osteoarthritis is unclear. Although the excess load placed on joint surfaces will accelerated the breakdown of cartilage, obesity is also correlated with osteoarthritis of the hand, indicating a more systemic cause. Obesity increases the chances of having metabolic syndrome. Metabolic syndrome is a condition characterized by a set of risk factors which are linked to coronary artery disease, stroke and type 2 diabetes. The risk factors include high blood pressure, abdominal obesity (fat around the waist), abnormal cholesterol levels (such as high triglyceride levels & low HDL levels) and insulin resistance (which corresponds with high blood sugar). The underlying theories of metabolic syndrome are tied to the body’s metabolism, most likely insulin resistance. Insulin resistance is the cells inability to efficiently use insulin, a hormone which transports sugar from the bloodstream to the cells. The result is high blood sugar. Insulin resistance is correlated to weight gain and inactivity.
In a recent study in the journal Skeletal Radiology, popliteal artery wall thickness was evaluated in individuals with osteoarthritis. Forty-two patients who were diagnosed with osteoarthritis at multiple joints were compared to 27 patients without osteoarthritis (the control group). An MRI of the knee was used to evaluate vessel wall thickness of the popliteal artery. The osteoarthritis group had thicker vessel walls than the control group, even when the researchers made adjustments for gender, weight and age. Because vessel wall thickness is directly related to high blood pressure and peripheral and coronary artery disease, the authors suggest that osteoarthritis might be another facet of metabolic syndrome.
One theory to explain the link between osteoarthritis and metabolic syndrome is based on white blood cells, immune fighting cells, increasing in areas where fat accumulates, especially around the abdomen (abdominal obesity). As the white blood cells increase, they contribute to widespread inflammation in the body, causing a pro-inflammatory state (as indicated by high blood levels of C- reactive protein) and the production of immune chemicals (specifically cytokines) which cause a chain reaction resulting in damage to the cartilage. The combination of insulin resistance and the pro-inflammatory state may also affect the normal cartilage repair process.
It is possible that osteoarthritis might be an inevitable outcome for those with metabolic syndrome.
Kornaat PR et al. Positive association between increased popliteal artery vessel wall thickness and generalized osteoarthritis: is OA also part of the metabolic syndrome? Skeletal Radiol. 2009 Jul 3.
Rojas-Rodríguez J, et al. The relationship between the metabolic syndrome and energy-utilization deficit in the pathogenesis of obesity-induced osteoarthritis. Med Hypotheses. 2007; 69 (4): 860-8.
Cicuttini FM, Baker JR, Spector TD: The association of obesity with osteoarthritis of the hand and knee in women: a twin study. J.Rheumatol. 1996; 23: 1221-1226.
Felson DT: Weight and osteoarthritis. J.Rheumatol. 1995; 43: 7-9.
Armstrong CG, Mow VC. Variations in the Intrinsic Mechanical Properities of Human Articular Cartilage with Age, Degeneration, and Water Content. JBJS. 1982; 64: 88-94.